Managing Pain With…Anthrax?!
By Laura Tran, C2ST Intern, Rush University
Imagine you are cooking and you accidentally touch a hot pot on the stove. Ouch! It happens in an instant. You pull your hand away as a reflex and then you feel the pain. Our sensation of pain comes from these receptors called “nociceptors”¹ (“no-see-septors”) that respond to stimuli such as temperature (e.g., hot or cold), mechanical pressure (e.g., stretch/strain), and chemicals (e.g., toxins/poisons). The heat from the pot is the stimulus that activates your nociceptors.
Nociceptors send chemical signals (neurotransmitters) to the spinal cord and travel to the brain. There, your brain can either release natural painkillers called endorphins, neurotransmitters that enhance pain, such as glutamate, or hormones like prostaglandins that stimulate our body’s immune system in response to an injury. This process happens naturally for everyone, although differing amounts of these neurotransmitters can influence how some people experience pain. This is why some people experience pain more intensely than others!
Pain can generally be categorized as acute or chronic. Acute pain tends to resolve itself once the affected area heals, like burning yourself while cooking. Chronic pain tends to last for much longer (months to years) and can either be intermittent or constant. Chronic pain is commonly treated with opioids². These are regarded as one of the most effective drugs for treating pain, however, opioid usage comes with a major caveat. Generally, opioids are not recommended for long-term use because the body can develop a dependence on the drug making it highly addictive.
Recently, scientists may have found an alternative treatment for pain that involves the toxins made from the bacterium Bacillus anthracis (B. anthracis).
That’s right. Toxins from B. anthracis, the bacterium known to cause anthrax, can “silence” multiple types of pain. A study³ from a group of scientists at Harvard Medical School has shown that certain components of anthrax toxin can alter signaling in our pain-sensing cells.
The pain-sensing cells that these scientists studied are referred to as dorsal root ganglion (DRG) sensory neurons. This is because nociceptor cell bodies mainly reside in the DRG of the spine. This is where pain signals from our environment, like those from our hot pot scenario, go. Thus, the DRG is an integral part of the process of feeling and reacting to pain.
Interestingly, researchers have found that some of our cells have receptors for anthrax toxins. Anthrax toxins⁴ are composed of three proteins: protective antigen (PA), edema factor (EF), and lethal factor (LF). These proteins can then combine to make up two-part toxins: lethal toxin (LT), composed of PA and LF, and edema toxin (ET), composed of PA and EF.
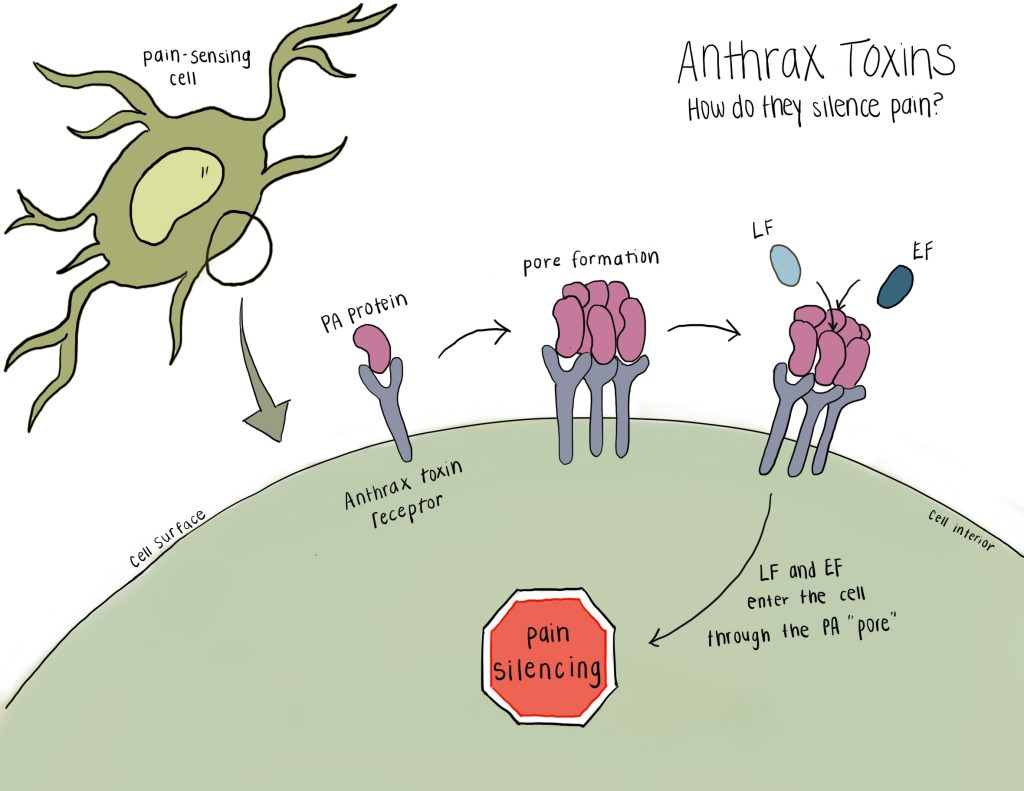
When anthrax toxins are present in the body, PA is the first protein to arrive by binding to the anthrax receptor (ANTXR2). Then, PA forms an opening (or “pore”) for both EF and LF to enter the pain-sensing cells. Once inside the cell, the anthrax toxins alter signaling to act as an analgesic, to relieve and reduce pain.
Researchers have shown that the anthrax toxin affects pain signaling in both human nerve cells as well as in mice. Mice, after having the toxin injected into their lower spines, could no longer sense extreme temperatures (hot and cold), mechanical stimulations (putting pressure on their paws), and pain caused by different models (inflammatory and neuropathic). Another important finding from this study was that the toxin did not produce major side effects, such as changes in heart rate, body temperature, and motor function. This shows how selective this treatment can be.
Researchers also modified the anthrax toxin to serve as a protein vehicle to successfully deliver different types of molecular cargo into pain-sensing neurons. One example of the cargo is botulinum neurotoxin, derived from another bacterium Clostridium botulinum (C. botulinum), which is also used in pain management⁵. The anthrax vehicle successfully ferried this neurotoxin into pain-sensing cells to block pain. Imagine the endless possibilities in effectively silencing pain!
Overall, the use of anthrax toxins as a targeted pain management treatment may be able to outcompete existing analgesics, especially since it appears that there are no negative side effects. Beyond the anthrax toxins acting as pain blockers themselves, the anthrax toxin vehicle system also has potential therapeutic value by delivering cargo into pain-sensing cells for synergistic effects. This can be a major game-changer in non-opioid pain treatment!
References: